Varicose veins are veins that have become enlarged and twisted. The term commonly refers to the veins on the leg, although varicose veins can occur elsewhere.
Veins have pairs of leaflet valves to prevent blood from flowing backwards (retrograde flow or venous reflux). Leg muscles pump the veins to return blood to the heart (the skeletal-muscle pump), against the effects of gravity. When veins become varicose, the leaflets of the valves no longer meet properly, and the valves do not work (valvular incompetence). This allows blood to flow backwards and they enlarge even more. Varicose veins are most common in the superficial veins of the legs, which are subject to high pressure when standing. Besides being a cosmetic problem, varicose veins can be painful, especially when standing. Severe long-standing varicose veins can lead to leg swelling, venous eczema, skin thickening (lipodermatosclerosis) and ulceration. Life-threatening complications are uncommon, but varicose veins may be confused with deep vein thrombosis, which may be life-threatening.

Varicose veins on a leg
Non-surgical treatments include sclerotherapy, elastic stockings, leg elevation and exercise. The traditional surgical treatment has been vein stripping to remove the affected veins. Newer, less invasive treatments which seal the main leaking vein are available. Alternative techniques, such as ultrasound-guided foam sclerotherapy, radiofrequency ablation and endovenous laser treatment, are available as well. Because most of the blood in the legs is returned by the deep veins, the superficial veins, which return only about 10% of the total blood of the legs, can usually be removed or ablated without serious harm.
Secondary varicose veins are those developing as collateral pathways, typically after stenosis or occlusion of the deep veins, a common sequel of extensive deep venous thrombosis (DVT). Treatment options are usually support stockings, occasionally sclerotherapy and rarely, limited surgery.
Varicose veins are distinguished from reticular veins (blue veins) and telangiectasias (spider veins), which also involve valvular insufficiency, by the size and location of the veins. Many patients who suffer with varicose veins seek out the assistance of physicians who specialize in vein care or peripheral vascular disease. These physicians include vascular surgeons, phlebologistsor interventional radiologists.
Signs and symptoms
- Aching, heavy legs (often worse at night and after exercise).
- Appearance of spider veins (telangiectasia) in the affected leg.
- Ankle swelling, especially in the evening.
- A brownish-yellow shiny skin discoloration near the affected veins.
- Redness, dryness, and itchiness of areas of skin, termed stasis dermatitis or venous eczema, because of waste products building up in the leg.
- Cramps may develop especially when making a sudden move as standing up.
- Minor injuries to the area may bleed more than normal or take a long time to heal.
- In some people the skin above the ankle may shrink (lipodermatosclerosis) because the fat underneath the skin becomes hard.
- Restless legs syndrome appears to be a common overlapping clinical syndrome in patients with varicose veins and other chronic venous insufficiency.
- Whitened, irregular scar-like patches can appear at the ankles. This is known as atrophie blanche.
Complications
Most varicose veins are reasonably benign, but severe varicosities can lead to major complications, due to the poor circulation through the affected limb.
- Pain, tenderness, heaviness, inability to walk or stand for long hours, thus hindering work
- Skin conditions / Dermatitis which could predispose skin loss
- Skin ulcers especially near the ankle, usually referred to as venous ulcers.
- Development of carcinoma or sarcoma in longstanding venous ulcers. Over 100 reported cases of malignant transformation have been reported at a rate reported as 0.4% to 1%.
- Severe bleeding from minor trauma, of particular concern in the elderly.
- Blood clotting within affected veins, termed superficial thrombophlebitis. These are frequently isolated to the superficial veins, but can extend into deep veins, becoming a more serious problem.
- Acute fat necrosis can occur, especially at the ankle of overweight patients with varicose veins. Females are more frequently affected than males.
Investigations
Traditionally, varicose veins were investigated using imaging techniques only if there was a clinical suspicion of deep venous insufficiency, if they were recurrent, or if they involved the saphenopopliteal junction. This practice is not now widely accepted. Patients with varicose veins should now be investigated using lower limbs venous ultrasonography. The results from a randomised controlled trial on patients with and without routine ultrasound has shown a significant difference in recurrence rate and reoperation rate at 2 and 7 years of follow-up.
Stages
According to the CEAP classification:
- C0 –no visible or palpable signs of venous disease
- C1 – telangectasia or reticular veins
- C2 –varicose veins.
- C3 –edema
- C4a –pigmentation or eczema
- C4b –lipodermatosclerosis, atrophie blanche
- C5 –healed venous ulcer
- C6 –active venous ulcer •Each clinical class is further characterised by a subscript depending upon whether the patient is symptomatic (S) or asymptomatic (A) e.g. C2S
Causes
Varicose veins are more common in women than in men, and are linked with heredity. Other related factors are pregnancy, obesity, menopause, aging, prolonged standing, leg injury and abdominal straining. Varicose veins are unlikely to be caused by crossing the legs or ankles. Less commonly, but not exceptionally, varicose veins can be due to other causes, as post phlebitic obstruction or incontinence, venous and arteriovenous malformations.
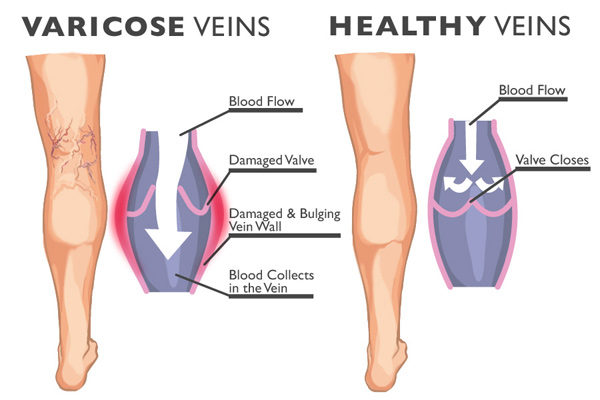
Varicose veins and healthy veins
More recent research has shown the importance of pelvic vein reflux (PVR) in the development of varicose veins. Hobbs showed varicose veins in the legs could be due to ovarian vein reflux and Lumley and his team showed recurrent varicose veins could be due to ovarian vein reflux. Whiteley and his team reported that both ovarian and internal iliac vein reflux causes leg varicose veins and that this condition affects 14% of women with varicose veins or 20% of women who have had vaginal delivery and have leg varicose veins. In addition, evidence suggests that failing to look for, and treat pelvic vein reflux can be a cause of recurrent varicose veins.
There is increasing evidence for the role of incompetent Perforator veins (or “perforators”) in the formation of varicose veins and recurrent varicose veins.
Varicose veins could also be caused by hyperhomocysteinemia in the body, which can degrade and inhibit the formation of the three main structural components of the artery: collagen, elastin and the proteoglycans. Homocysteine permanently degrades cysteine disulfidebridges and lysine amino acid residues in proteins, gradually affecting function and structure. Simply put, homocysteine is a ‘corrosive’ of long-living proteins, i.e. collagen or elastin, or lifelong proteins, i.e. fibrillin. These long-term effects are difficult to establish in clinical trials focusing on groups with existing artery decline. Klippel-Trenaunay syndrome and Parkes-Weber syndrome are relevant for differential diagnosis.
Another cause is chronic alcohol consumption due to the vasodilatation side effect in relation to gravity and blood viscosity.





